Using Your Benefit Convenience Card
Summary
Healthcare Cost Assistance benefits cover 100% of your net monthly premiums for your individual Marketplace plan. These benefits also provide funds for out-of-pocket medical expenses for claims covered by Medicare or your approved Marketplace plan.
You manage these benefits with your Benefit Convenience Card (BCC). The BCC is a Mastercard credit card, sent to you and administered by Ameriflex.
Your BCC works just like a regular credit card, except that:
- Your card is limited in use to Marketplace premium payments and covered out-of-pocket medical expenses. Covered medical expenses include deductibles, copayments, and coinsurance expenses, such as covered prescriptions. Please see the Summary of Benefits for your plan here.
- Since the BCC is only for covered medical expenses, you may need to show proof of your covered out-of-pocket expenses. Please keep your Explanation of Benefits (EOBs) and receipts. It’s especially important to keep your prescription receipts, since prescription expenses don’t appear on the EOBs issued by your insurance company.
The BCC can’t be used for:
- Premium or out-of-pocket expenses for dental, vision, and/or hearing services.
- ATM withdrawals or to get cash back when making a purchase.
- Expenses for your spouse or dependents.
- Expenses for products or services that your health insurance plan doesn’t cover.
- Premium expenses to anyone other than your current medical carrier.
- Expenses incurred while you were not eligible for Healthcare Cost Assistance benefits.
- Covered medical expenses from a previous calendar year; for these expenses submit a reimbursement request by filling out the Ameriflex Reimbursement Claim Form online.
- Your individual premium payment if your family is on the same premium bill; for your individual premium payment, submit a reimbursement request through MyCarewellSEIU503 or by filling out the Medical Premium Reimbursement Claim Form online.
You may be financially responsible for repaying funds to Carewell SEIU 503 if your card is used for expenses that are not covered medical expenses.
One of the best things about the BCC is that you can set up autopay and make sure your premium is paid on time every month.
Contact your insurance carrier to set up automatic payments from your Benefit Convenience Card:
- Kaiser: Visit the Kaiser Permanente website.
- PacificSource: Visit the PacificSource website.
- Moda: Call Moda customer service at 1-503-243-3962 or toll-free at 1-877-605-3229, identify yourself as a homecare worker, and let them know you want to set up recurring automatic payments.
- Providence: Call Providence billing at 1-503-574-5791 or pay your premium online — for first time premium payments, use this link and select New individual & family applicants.
- Regence: Customer Service 1-888-675-6570 / Regence website / To create an account, go to www.regence.com/member/registration.
What can you use the Benefit Convenience Card for?
Monthly premiums |
Out-of-pocket expenses |
|
|---|---|---|
Approved Marketplace Plan |
Monthly premiumsYES! [Exceptions may apply, see below] Contact your insurance carrier to set up your card to make automatic premium payments. |
Out-of-pocket expensesYES! Covered medical expenses (up to the annual BCC allowance): – The deductible on your approved Marketplace plan – Copayments and coinsurance expenses, including for covered prescriptions
|
Medicare |
Monthly premiumsNO. You will need to use the reimbursement process for your Medicare premium(s). Click here for more information. |
Out-of-pocket expensesYES! Covered medical expenses (up to the annual BCC allowance): – Deductibles on your Medicare coverage – Copayments and coinsurance expenses, including for covered prescriptions |
Exceptions
- If your family is included on your health insurance policy, or
- If you receive the temporary Healthcare Cost Assistance benefit
In both cases, you may still use the BCC for covered out-of-pocket expenses. However, you must pay your premium directly to your insurance company using your own funds and then submit a Medical Premium Reimbursement Claim Form to Carewell SEIU 503. Once your reimbursement request has been processed, you will receive a check for the amount of your premium.
How much money is on the BCC?
There are two separate accounts on your BCC: one for paying your premiums (if applicable), and one for covered out-of-pocket expenses.
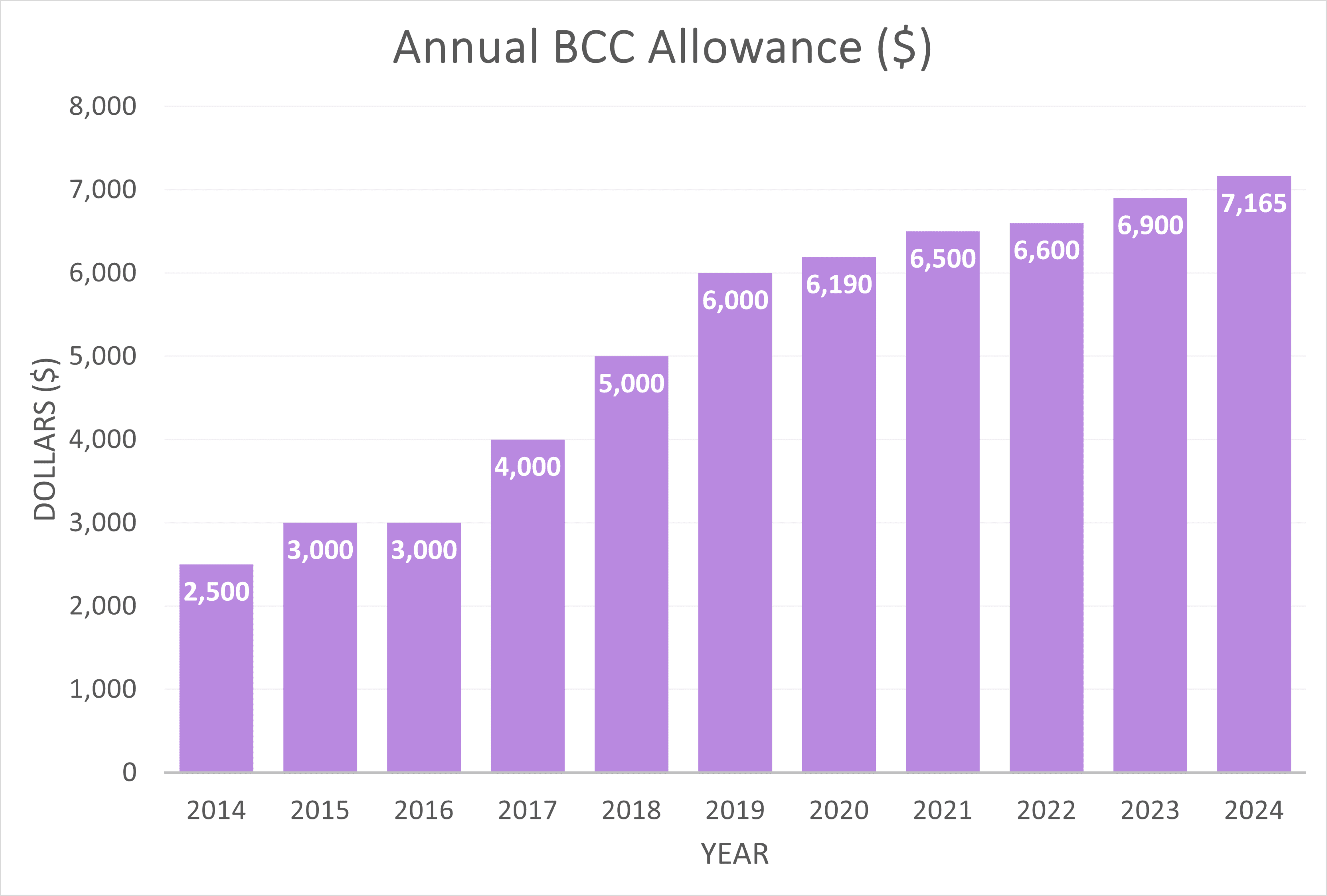
This chart shows the amount available for the annual BCC allowance for covered out-of-pocket expenses since the start of this program.
Submit a claim for reimbursement from Ameriflex (BCC Administrator)
Submit a claim for reimbursement from Ameriflex:
-
- Covered Medical out-of-pocket expenses if you paid with your own funds.
- Covered Medicare out-of-pocket expenses if you paid with your funds.
- Medical monthly premium – net monthly premium for qualifying individual plans purchased through the Marketplace (not family plan, not temporary Healthcare Cost Assistance reimbursement).
- For reimbursement for services received the previous year, submit a reimbursement form to Ameriflex for services received up to 12 months back, if you were eligible for Healthcare Cost Assistance at the time.
- For expenses over $80, you are required to submit proof. Please keep your Explanation of Benefits (EOBs) and all receipts (especially your prescription receipts since prescription expenses do not appear on the EOBs issued by your insurance company).
Connect with Ameriflex!
Managing your Benefit Convenience Card issued by Carewell SEIU 503 just got easier! For all your transactions with Ameriflex, we highly recommend you create an account on the Ameriflex portal. You can use the Ameriflex online portal at ameriflex.wealthcareportal.com to:
-
- check the balance on your Benefit Convenience Card (BCC)
- view your payment history
- submit claims online
- see the status of a reimbursement
- order a replacement card
3 steps to make managing your BCC payments easier
Create an Account
Create your account at ameriflex.wealthcareportal.com.
Set up and use MyPlanConnect.
If you use your BCC, MyPlanConnect will automatically locate the Explanation of Benefits (EOB) for your transaction, and you won’t need to submit further documentation.
See details and directions at https://myameriflex.crunch.help/participants/Setting-Up-and-Using-MyPlanConnect.
Download App
Once you’ve set up your account, download the MyAmeriflex mobile app at myameriflex.com/participants/the-ameriflex-difference/mobile-app. The Ameriflex app lets you access and manage your account on the go!
Ameriflex resources
Accessing the Ameriflex portal and MyPlanConnect
Accessing the Ameriflex Mobile App
Other Ameriflex resources
Contact Ameriflex
Ameriflex representatives are also available to assist on the phone Monday through Friday 5am to 6pm, and Saturday 7am to 11am (PST) at 1-888-868-3539.